Will West, who was a resident in ophthalmology, performs an eye procedure in 2023.
15:59 JST, October 8, 2024
David West barely slept the night his older brother, William Ballantyne West Jr., called him from his D.C. apartment, sounding worried.
His brother had earned the nickname “Iron Will” for the tenacity he showed when faced with challenges. He had rock-climbed, gone on a religious mission to Italy and competed in overnight relay races. But during that call earlier this year, Will talked about how his problems felt too big to solve: He was not getting the training he needed to prepare him to practice medicine. He was not getting enough time to sleep or recharge after long shifts. Happiness, he felt, would elude him always.
Will was a doctor in his third year of ophthalmology surgical training at George Washington University School of Medicine and Health Sciences in D.C., and David, six years younger and following the same path, was in his first year of medical school in Utah.
David considered asking someone to check on his brother, but during their next two phone calls, Will eased his concerns. He laughed and seemed lighter. After a call in late February, David hung up feeling relieved.
Days later, Will was gone. He died by suicide at the age of 33.
There is no way to know for certain what led Will to end his life. But what is known, interviews with Will’s family, George Washington residents and national experts show, is that despite a growing acceptance nationwide of the benefits of mental health care, barriers persist in residency programs that keep doctors from seeking help during a time when many need it.
Many factors, experts say, make doctors at that high-stress, high-stakes stage in their careers vulnerable. Residents – medical school graduates who spend three to seven years training in their specialty under the supervision of attending physicians – can face grueling 80-hour workweeks on modest salaries. They can also feel compelled to hide their struggles, fearing the repercussions that disclosure might bring. Success in their programs is critical to landing the jobs that will launch their careers.
Will’s family believes the pressures of residency kept him from seeking the mental health treatment he needed. The questions that pull at them now: How many other residents are on the precipice of making the same choice, and whether changing the culture of programs across the nation can help them before it’s too late.
Will wrote two letters before he died.
He addressed one to his brother. At Will’s request, David has chosen to keep that one mostly private.
Will opened the other letter “Hello All.” His family shared that one with The Washington Post, because it holds a warning for other residents and those who oversee them.

Will West, seen here in 2021, was in his third year of residency at George Washington University when he died by suicide.
Who cares for the healers?
The question of who cares for the healers plagued medicine long before Lorna Breen, an emergency department physician in New York City, died by suicide in 2020. But her death amplified the mental health crisis among doctors.
The chaos of covid-19 shook Breen, leaving her unable to function as she once had and prompting her family to arrange for friends to transport her from New York to a Charlottesville psychiatric unit. From her hospital bed at University of Virginia Medical Center, she said she feared the treatment would cause her to lose her medical license, her brother-in-law, J. Corey Feist, said.
Days after being discharged, she ended her life.
Doctors who receive mental health care may have to report it when they apply for jobs, medical licenses or insurance. The uncertainty of how that information will reflect on them can leave many hesitant to seek help, said Stefanie Simmons, chief medical officer at the organization Feist co-founded in Breen’s name, the Dr. Lorna Breen Heroes’ Foundation.
“You are facing the decision of whether to put your future career, which is often your mission in life to care for others and use your talents to do that, at jeopardy by taking care of yourself in a way that you know you should be,” Simmons said.
The foundation advocates for states, hospitals and health systems to change disclosure forms so that they either ask nothing about mental health, ask one question that treats mental and physical health the same or ask applicants to attest to proactively caring for themselves.
Christine Moutier, chief medical officer at the American Foundation for Suicide Prevention, said graduate program leaders have worked hard in the past decade to address the challenges that keep residents from seeking mental health treatment, but reforms have been instituted unevenly and stigmas persist.
It helps, she said, for residents to have strong relationships with mentors and regular check-ins to process not only medical lessons but the feelings that come with bad clinical outcomes, lack of sleep and conflicts with other residents or administrators.
The need for change, experts say, exists at medical institutions across the country. That means Will’s struggles at George Washington were not unique. But his death has brought into painful focus the need to prioritize mental health among physicians and to do so with urgency.
Will didn’t seek mental health care while at George Washington, even though he had experienced depression for much of his life and had been diagnosed with attention-deficit/hyperactivity disorder (ADHD), his brother David said.
It wasn’t because Will didn’t believe in the power of therapy. He had used mental health services in medical school in Utah, David said. His brother, he said, feared that seeking help in residency would torpedo a career and life he had been working toward for as long as he could remember.
“Imperfection is not allowed,” David said of his brother’s residency experience. “Weakness is not either. When it’s there, it’s treated with disdain instead of an opportunity for learning and growth.”
In interviews with The Washington Post, several residents at George Washington, who spoke on the condition 0f anonymity because of fear of retaliation, described feeling trapped in a stressful environment where some degree of depression seemed almost normal, causing doctors to go through the motions, lose interest in hobbies and count the minutes until they could leave the clinic to go home and be alone.
George Washington administrators, through spokeswoman Julia Metjian, declined to answer specific questions about Will’s death or its residency programs but provided a general statement.
“The safety and well-being of GW students, faculty, and staff – including our residents – is the university’s highest priority,” the statement said.
“At GW, like other medical training programs, we recognize that the residency experience can be personally challenging and that residents may need professional support for their well-being,” the statement said. “The GW School of Medicine and Health Sciences (SMHS) offers resources to support the physical, emotional/mental health, and overall well-being of residents – including confidential counseling at no cost.”
‘A true life and death battle’
On a yellow Post-it note, Will wrote “emergency contact” followed by his father’s name and phone number. He then placed that on a sheet of loose-leaf paper covered front and back with his final words in neat script.
The letter begins: “I apologize that this is the best I can do for goodbye. Many of you deserve better but one can’t exactly talk much about this kind of thing in advance so a note will have to do.”
He explained that no recent event played into his decision. He then wrote:
“To those who will be negatively affected by my actions, I’m so sorry. I have simply run out of gas and have nothing left to give.
To those in a position of authority over residents, a simple reminder that we come to you seeking the possibility of a better life. Some of us with challenges you do not see or backgrounds of which you are not aware.”
When Will was a skinny ninth-grader, he got knocked to the ground at the crowded starting line of a 5-kilometer road race. He stood up cradling his arm and in tears, and he finished the race that way. When he went to the doctor afterward, he found out that he had fractured his collarbone.
“That was one of the first times I remembered thinking, ‘This kid is tough.’ From a young age he was just driven, and he never stopped, no matter what,” said Michael Christensen, Will’s friend of 20 years.
Will helped Christensen move from Utah to Albuquerque in the middle of December for his physician assistant training. One hour into the 10-hour drive, they came upon an icy summit and found a car facing the wrong way after skidding on the slick highway. A pregnant woman had been thrown into a snowbank and her husband was bleeding from the neck with his head plunged through the windshield, Christensen said.
“Will ran over to the guy in the car and put his hand straight on the guy’s jugular to stop the bleeding,” Christensen recalled. When paramedics arrived an hour later, Will gave them a report. “Will just kept his head cool the entire time.”
They later learned the couple survived.
Will could concentrate for hours making quilts and elaborate gingerbread houses with his sister Lucy, but he also loved long-distance overnight relay races and watersports. He purchased an ambulance and retrofitted it as a roaming home while in medical school at the University of Utah.
At George Washington, his mental health took a “significant downturn,” his family said. He went through a breakup with his girlfriend and he was plagued by self-doubt. His family recalled him asking: Do people think I’m lazy? Will I be able to compete for the jobs I want? Will I be competent if hired? Will I be able to treat patients safely on my own?
Better access to mental health resources, such as regular appointments with a provider and access to medication without fear of reprisal could have helped dramatically, David said. At times, his family considered calling the school to insist he get help.
At her son’s funeral, Lisa West spoke of having regrets and told the hundreds who gathered in the Church of Jesus Christ of Latter-day Saints chapel that she knew many of them had some, too.
“He was fiercely independent, private, determined and stubborn,” she told those gathered. “And it’s possible that if we did everything humanly possible that we wanted to, he could have still been in this place.”
Will’s letter continued:
“There are other residents right now fighting a true life and death battle – one that is waged both inside and out at the clinic/hospital. Often that battle may cause symptoms that look an awful lot like laziness, lack of motivation or waste of intelligence, all unforgivable sins in our profession.”
‘How many more residents have to die?’

About 75 residents held a rally in May on the campus of George Washington University to draw attention to union demands for better working conditions.
Three months after Will’s death, about 75 residents, many wearing scrubs and white coats, finished shifts at George Washington University Hospital and walked to the courtyard outside the medical school to rally for a mental health stipend and better salaries and hours.
They had also come with Will on their minds.
They bowed their heads in a moment of silence for him.
Some of those who gathered held signs reading: “How many more residents have to die?” “Fair wages save lives,” “Overworked & Underpaid” and simply “I’m tired.”
Maryssa Miller, an internal medicine resident who emceed the rally, said working 80 hours per week with scant time for herself crippled her mental health.
Every day she called her mother at 5 a.m. on the way to work, crying, and on the way home the following day, crying. She lost 20 pounds.
“It just seemed like there was no out and it could never get better,” she said.
Finally, Miller prescribed herself an antidepressant “that saved me,” she said.
Another rallygoer, Elsa Alaswad, a neurology resident, said she couldn’t obtain regular therapy appointments through the school’s offerings and it took nearly two years to find a provider who was taking new patients and would accept her insurance.
Although she wasn’t close with Will, she said he made it known he needed help: “He didn’t have a lot of the support he should have and he felt isolated.”
George Washington Hospital, where hundreds of residents work, serves the greater Capital region, meaning doctors treat low-income patients and political VIPs at a trauma center six blocks from the White House.
Doctors affiliated with George Washington will also staff a new hospital, Cedar Hill Regional Medical Center, set to open next year in medically underserved Ward 8.
The residents say their well-being is critical to keeping the community healthy and the need for mental health resources helped fuel their decision last year to form a union, an effort Will supported.
Five current and former residents who worked with Will described a high-pressure culture where supervising doctors relied on the Socratic method and would call out mistakes publicly.
They said Will was talented, hardworking and empathetic, but that he was among those critiqued as he pushed back against a system that didn’t always make sense to him.
Will also seemed to take to heart the plot of the 1949 film, “Twelve O’Clock High,” in which a general takes command of a World War II bomber unit. Ophthalmology residents watch it as part of a lesson on leadership. His mother later found a note he wrote on his phone about the film. It read: “the weak link kills himself.”
Shortly before his death, residents said, Will bristled at an on-call system based on seniority that he considered unfair, to the frustration of some of his colleagues. They were all trying to get through a challenging time. It didn’t occur to them, the residents said, that he was in trouble.
“I thought he would graduate,” one resident said. “I thought he would get through it.”
‘Wish you all the very best’
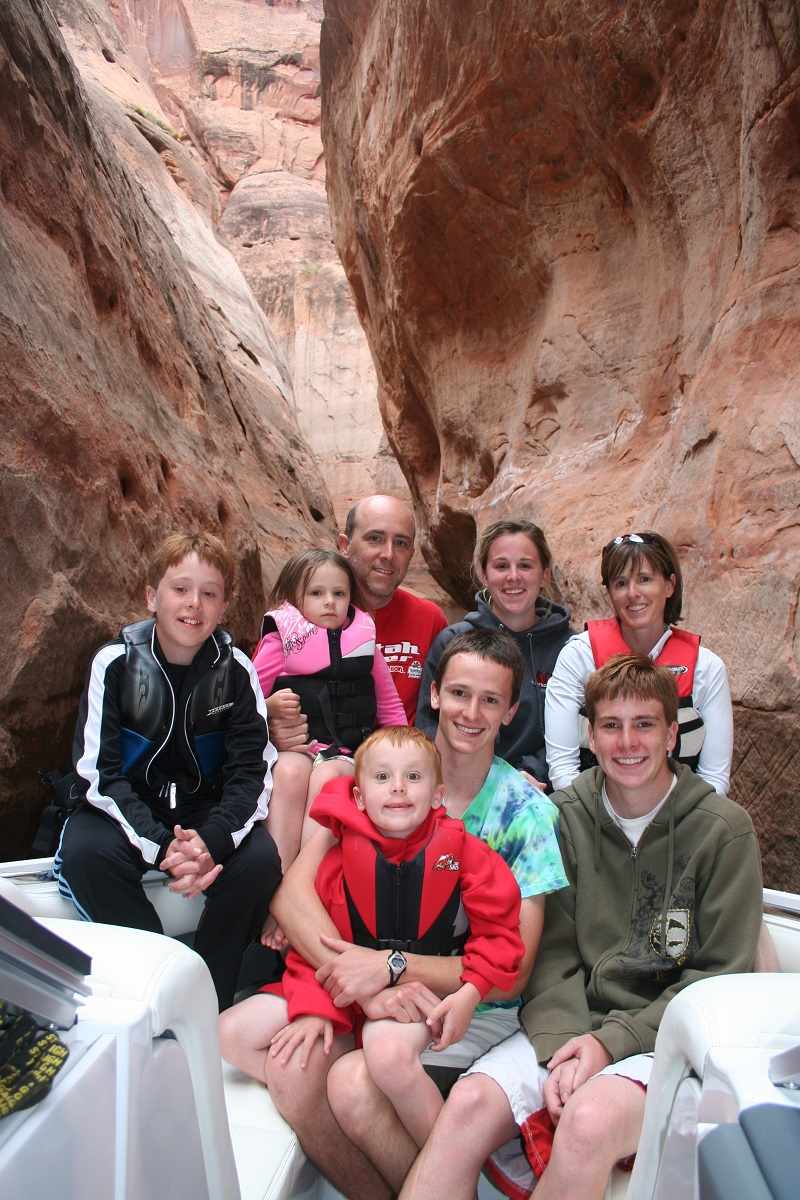
Will West Sr. and his wife Lisa West went to Lake Powell in 2009 with their six children. Back row, from left, David, Lucy, Will Sr., Jennifer and Lisa. In the front row, left to right, are George, Will and Peter.
Will West Sr. received the call on a Friday evening in March. The D.C. police had found his son’s lifeless body in his apartment after a welfare check.
The family soon pieced together Will’s final days. He had taken a sick day. He had emptied his bank account, putting aside the money for David. In one of his final calls to his brother, Will asked after each of their siblings. David said it dawned on him later that Will wanted to make sure they’d be okay without him.
After his death, his parents flew to D.C. to clear out his apartment and arrange to bring his body home. They met with graduate program leaders whom they felt dismissed Will’s death. They returned to D.C. a month later, hoping medical leaders would see Will’s suicide note as a call to action.
In an email sent to George Washington’s medical community three days after Will’s death, officials shared a list of resources, including an Employee Assistance Program that offers up to five counseling sessions, Talkspace, an online therapy platform where patients can text a therapist, and Headspace, a mindfulness app.
In the statement the university sent to The Post, academic leaders pledged that all first-year residents, beginning this fall, will be scheduled for an introductory appointment with the campus’s Resiliency & Well-Being Center.
“The university is aware of and strives to eliminate the culturally entrenched stigma that has long interfered with physicians’ willingness to seek help with, at times, life-threatening mental conditions,” according to the statement.
The West family has asked leaders to institute reforms, including built-in therapy sessions and a schedule that allows time for mental health care. They are also preparing a list of detailed recommendations, including regular self-care training. And they plan to share their son’s story at upcoming national conferences.
“The battle is just beginning,” Will West Sr. said.
At his funeral, his mother, dressed in yellow to honor Will’s vibrant spirit, recounted her grief: She was angry. She threw things. She asked herself, how could this happen? How could it have been allowed to happen?
After a sleepless night, numb and in despair, she sought solace at the Mormon Temple. Will’s passing was a test of her faith, she said. Her faith fuels her belief that she will see her son again and that his death will lead to progress for others.
That hope drives her to seek change. Her son, she believes, wanted that, too.
His letter continues:
“I hope that an effort can be made to understand, support, and mentor the residents rather than simply to assess and drive them toward their highest potential as doctors.
To be clear, there are other people at real risk here at GW.”
He signs off with kind words for his friends and mentors:
“Thank you so much for being there for me. I wish you all the very best.
Sincerely,
Will West”
Top Articles in News Services
-

Survey Shows False Election Info Perceived as True
-

Hong Kong Ex-Publisher Jimmy Lai’s Sentence Raises International Outcry as China Defends It
-

Japan’s Nikkei Stock Average Touches 58,000 as Yen, Jgbs Rally on Election Fallout (UPDATE 1)
-

Japan’s Nikkei Stock Average Falls as US-Iran Tensions Unsettle Investors (UPDATE 1)
-

Trump Names Former Federal Reserve Governor Warsh as the Next Fed Chair, Replacing Powell
JN ACCESS RANKING
-

Producer Behind Pop Group XG Arrested for Cocaine Possession
-

Japan PM Takaichi’s Cabinet Resigns en Masse
-

Man Infected with Measles Reportedly Dined at Restaurant in Tokyo Station
-

Israeli Ambassador to Japan Speaks about Japan’s Role in the Reconstruction of Gaza
-

Videos Plagiarized, Reposted with False Subtitles Claiming ‘Ryukyu Belongs to China’; Anti-China False Information Also Posted in Japan