Daniel Gade said a presidential panel he served on made inconsequential changes to the disability benefits systems.
12:47 JST, November 11, 2025
Over decades, the government has spent billions on disability payments for veterans with sleep apnea, a common condition that interrupts breathing during sleep and causes fatigue. In early 2022, officials were determined to pare that back.
Medical advances mean most apnea sufferers now have few or no symptoms and can hold jobs. So Denis McDonough, then the secretary of the Department of Veterans Affairs, announced a proposal to change the benefits system to reflect the new reality, and – going forward – slash monthly checks for many veterans.
It went nowhere.
The episode was the latest failed attempt to rein in the $193 billion disability program in the era of modern medicine. Even as once-debilitating ailments become manageable for most patients, the government has repeatedly backed away from updates that would anger veterans and their supporters, The Washington Post found.
Approved sleep apnea claims have exploded, growing more than elevenfold from 2009 to 2024, VA data shows. Last year, about 660,000 veterans collected disability benefits for sleep apnea – up from 57,000 in 2009.
It’s created “a catch-22 all the way around,” said retired Army Lt. Gen. James Terry Scott, who led a presidential commission starting in 2004 to assess the disability system.
“The gist was things [the government] should do to get a grip on sleep apnea,” Scott said of his commission’s focus. “But people have learned the easy way out is to find in favor of the veteran.”
McDonough’s plan would substantially reduce payments for the condition, now typically $1,100 a month or higher – a larger sum than most veterans receive for a leg amputated below the knee. At a February 2022 news conference, the secretary said VA was modernizing its disability system, which had changed little since World War II.
McDonough also proposed more stringent standards for claims for tinnitus, a persistent ringing in the ears. New rules for mental health claims, including post-traumatic stress disorder, or PTSD, would require veterans to show how it affects their lives at home or at work.
Veterans and their advocates were furious. They flooded the Federal Register, which listed the proposed rule changes, with thousands of angry comments.
“I demolished my body for the country,” one veteran wrote. “And what does the country do for me? Things like this.”
The disability benefits system was meant to be a social safety net for returning service members whose combat wounds kept them from working. Today it is overrun with dubious and exaggerated claims that have little to do with military service, a Post investigation published in October found. VA approves millions of claims for common diseases of aging, including diabetes, and conditions related to high blood pressure and hardening of the arteries. A booming for-profit industry coaches veterans to exploit the system for bigger payouts, The Post found.
Benefits are granted based on a system that rates individual ailments on a scale from zero to 100 percent. Veterans often claim multiple conditions, combining these ratings until they reach 100 percent. That threshold – with its large payout and other perks such as property tax breaks, and free health and dental care – is hyped by for-profit claims consultants as “the holy grail.”
The vast majority of veterans awarded benefits for sleep apnea and prescribed treatment for it receive a disability rating of 50 percent for that condition alone, according to VA officials. In contrast, most veterans who have a leg amputated below the knee or blindness in one eye are rated at or below 40 percent.
Indira Gurubhagavatula, a professor of medicine at the University of Pennsylvania and sleep medicine specialist at the Philadelphia VA Medical Center, said veterans have become savvy on social media to the generous benefits for sleep apnea.
“The common question I get is, ‘Is this compensable or not?’” Gurubhagavatula said, noting that some veterans ask her to test them for it. “A lot of the time they tell me, ‘I know someone who got rated for this.’”
McDonough’s proposal would not affect the disability rating or compensation of veterans already receiving benefits for sleep apnea. But monthly payments would be slashed – often down to $0 – for new claims when symptoms are successfully treated.
At the time, VA officials were optimistic that there was political will to adjust the system.
“I’ve learned over the time that I’ve been in this role never to predict when a particular rule will be published, but I think we’re very, very close,” Joshua Jacobs, then VA’s undersecretary for benefits, said in an interview with The Post a few weeks before President Joe Biden left office.
But McDonough did not sign off on his own proposal before stepping down with the rest of the administration.
Through a spokesperson, he declined to comment on why he did not give the final green light. Jacobs also declined to comment.
Under the Trump administration, the plan is still pending almost four years later.
In recent months, the administration has signaled that it may implement some or all of the changes by the end of the year. In September, officials moved the proposal to the final rule stage in the Federal Register.
McDonough’s successor, Douglas A. Collins, was sworn in in February. He declined to be interviewed for this article.
Pete Kasperowicz, a VA spokesperson, did not respond to written questions about whether the department planned to change disability compensation for sleep apnea. In an emailed statement, Kasperowicz said VA has been in “the process of modernizing” the benefits system since the first Trump administration and plans to conclude the effort during the president’s second term.
Kasperowicz said VA is working on updates to “respiratory/ear-nose-throat,” “mental disorders” and “neurological conditions and convulsive disorders” – systems that include sleep apnea, PTSD and tinnitus, among other ailments.
“Once complete, this will be the first total update of the schedule since 1945,” he said in the email. He added, “While the far-left Washington Post’s objective is to smear disabled American Veterans as crooks and liars and cut their benefits, VA’s goal is precisely the opposite: We want to simplify access to VA benefits and health care and make it easier for Veterans to get what our nation owes them.”
As they wait to see what the government will do, veterans are filing a flurry of claims for sleep apnea benefits. The Veterans Benefits Administration, the division of VA that handles disability compensation, approved 150,000 more claims in 2024 than in 2022, VA data shows.
“It’s the most controversial condition right now,” said Michele Colpaert, a national service officer with Disabled American Veterans, a nonprofit group chartered by Congress that helps former service members claim benefits.
“Everyone wants to file for sleep apnea.”
Calls for action
Researchers estimate that about 30 million Americans suffer from sleep apnea, although only about 6 million have been officially diagnosed. In middle age, it affects almost 1 in 4 men and 1 in 10 women. Being male and overweight are both risk factors for apnea, making the condition more prevalent in the veteran population, although research varies on how much.
First identified as a medical condition in 1965, sleep apnea once was considered a dire diagnosis. Untreated, those who suffer from it often wake up gasping because their airway has collapsed, blocking the flow of oxygen into their lungs. The disorder can cause snoring, daytime drowsiness, high blood pressure and, in rare cases, heart failure or stroke.
The introduction in the 1980s of the commercially available continuous positive airway pressure machine, or CPAP, allowed the vast majority of apnea sufferers to find relief from their symptoms and lead normal lives. The bedside device sends a stream of air through a nasal mask and tube to keep the airway open, allowing people to wake up rested and work a normal day. The device also has been shown to reduce the risk of death and some medical conditions, including high blood pressure in those with severe apnea, research shows. It may also lower the risk of cardiovascular disease, said Gurubhagavatula, the Philadelphia sleep specialist.
VA added apnea to its list of ailments eligible for compensation in 1996, tying disability ratings to the severity of the disease. Veterans with mild symptoms are assigned a rating of 30 percent; those with life-threatening complications are designated 100 percent.
The government not only assigned apnea a high rating scale, but also made it relatively easy for veterans to get their claims approved. Unlike private insurers, VA grants benefits regardless of whether a veteran uses a CPAP machine or other device that offsets their symptoms or mitigates them entirely. And VA doctors are not required to follow up to verify that a veteran actually uses the CPAP or other prescribed treatment.
When the government created these rules nearly three decades ago, the CPAP was not as widely used or as effective at treating apnea as it soon became, said David Shulkin, a physician who served as VA secretary for close to 14 months during the first Trump administration.
As the field of sleep medicine grew, more doctors and clinics began offering breathing tests for apnea, and the CPAP became a household name, leading to a growth in claims, Shulkin said.
Federal officials and lawmakers began to question whether the disability benefits system was out of step with advances in medicine.
In 2004, at the height of the war on terror, President George W. Bush appointed a 13-member commission of retired senior military officials to conduct a reassessment. It was the first modern effort to examine the rating rules since they were developed in 1945.
In 1955, President Dwight D. Eisenhower became concerned about the growing cost of veterans’ care after the Second World War, when former service members and their families made up a large share of the U.S. population.
He appointed a commission led by five-star Army general and World War II hero Omar Bradley to recommend savings in the disability system and other benefits for veterans. In a 1956 report, the commission urged limiting benefits to only the most wounded and ill former service members. But pushback from veterans groups and politicians blocked any traction.
The Bush panel came back in 2007 with a 562-page report shared with Congress, the White House and VA leaders, urging an overhaul.
The report called on the government to provide better treatment and higher compensation to veterans with PTSD and traumatic brain injuries. It also emphasized that the disability rating system had not accounted for advances in science, medicine and technology, “as well as changes in the nature of work that have occurred in the past 62 years – which potentially affect the extent to which disabilities limit one’s earning capacity.”
“The intent was to modernize and get the subjectivity out of the claims review,” recalled Scott, the retired general who led the effort.
The commission recommended that VA conduct a broad review of the ratings it assigned to disabilities, including sleep apnea, to make sure they aligned with medical advances. Congress held hearings, and lawmakers pushed VA to follow through.
But little came of it. The wars in Afghanistan and Iraq had intensified; troops went on multiple deployments. The government turned its attention to helping soldiers returning with traumatic brain injuries and PTSD receive compensation and treatment, Scott said. Concerns about excesses in other areas were largely sidelined, he said.
In the following years, both the Government Accountability Office, Congress’s watchdog arm, and the VA inspector general’s office criticized the agency for neglecting to modernize the disability system. In 2008, Congress made the Bush disability commission permanent, with a mandate to advise the secretary on how the rating system could be brought into the 21st century.
In reality, the commission removed only a small number of obsolete disabilities – such as scurvy – and made other inconsequential changes, according to Daniel Gade, who served on the panel from 2008 to 2013.
Gade, a decorated Army officer who lost his right leg on a deployment to Iraq in 2004 and co-wrote the book “Wounding Warriors: How Bad Policy is Making Veterans Sicker and Poorer,” said the panel’s unstated goal was to boost ratings and disability payments.
“The only way that any benefit ever moves is in the direction of greater benefits,” Gade said in an interview. He recalled that the director of Disabled American Veterans told him at the time that “if one veteran loses one dollar [in the process of modernization] then DAV will be opposed.”
In an interview with The Post, Randy Reese – then a senior official with the veterans organization and now executive director of its Washington office – said he is opposed to any reductions in benefits for sleep apnea, because its symptoms, whether treated or not, can affect every part of a veteran’s life.
Some leg amputations, Reese said, are not as disabling.
“If you have a prosthetic leg, you can still work. There’s not a single case of sleep apnea that doesn’t affect your ability to work.”
‘Down the rabbit hole’
By President Barack Obama’s second term, the disability commission had become alarmed by an outsize growth in sleep apnea claims. VA data shows that from 2009 to 2012, awards for the condition had doubled from about 57,000 to 114,000 – and showed no sign of ebbing.
Sleep apnea has become more prevalent over several decades, in part because of rising rates of obesity, a known risk factor for developing the condition, according to recent research.
To receive disability benefits, a veteran must prove that their illness or injury is service-connected, meaning that it began or worsened during their time in the military. But if a veteran can show that an approved condition led to other health problems – even decades after leaving the service – VA will rate those ailments as “secondary” and award additional benefits.
In the case of sleep apnea, a “buddy letter” from another service member they served with or a spouse who can vouch for a history of snoring is sometimes enough to help a veteran prove the condition is service-connected.
During this time, service organizations and staffers who process disability claims say, tens of thousands of veterans began filing for sleep apnea, saying it resulted from the PTSD they were already rated for.
“Vets know it’s highly rated,” said Ryan Gallucci, executive director of the Washington office of Veterans of Foreign Wars, one of the oldest veterans service organizations chartered by Congress, of the spike in sleep apnea claims.
Gallucci acknowledged that “the perception can be that people are exaggerating,” and said he felt conflicted that some veterans receive benefits for apnea that developed years after they left the military. “You could say, ‘How far down the rabbit hole are we going?’”
The disability commission in 2014 called in a group of sleep experts for a briefing to address the surge in claims, Scott and Gade recalled.
Convinced that VA was being too generous with these claims, the commission sent an urgent recommendation to Allison Hickey, then the undersecretary for benefits. It suggested that VA lower the sleep apnea rating – and thus shrink monthly checks – for veterans whose symptoms improved with treatment.
Hickey declined to comment for this article. VA did not act on the recommendation at the time.
That year, the issue reached then-Sen. Tom Coburn (R-Oklahoma), an obstetrician who had become a powerful voice on government waste and spending. He scrutinized the growth in sleep apnea awards in the “Wastebook,” his annual compilation of federally funded programs that he said represented government waste.
“Exploding Claims of ‘Sleep Apnea’ Threaten to Bankrupt VA Disability Program,” read the “Wastebook” headline.
“Military personnel diagnosed with sleep apnea are given a 50 percent rating – and some believe it’s causing an explosion of abuse in the VA’s disability program,” Coburn wrote. “ … The VA itself has acknowledged the surge in sleep apnea claims, and taken steps to study the situation, but denies that there is any abuse in the system and defends the 50 percent rating. But critics allege the increase is nothing more than a scam on the VA disability system that takes resources away from veterans who are truly disabled.”
In 2016, nearly a decade after the Bush commission’s urging, the benefits administration began its review of the disability rating and compensation system. Officials promised to analyze every condition that was eligible for benefits and to recommend changes.
Federal watchdogs continued their drumbeat.
In 2020, the VA inspector general’s office found in an audit that almost half of the 250,000 veterans issued a CPAP or other device to treat sleep apnea from October 2016 through May 2018 used it less than half the time. Auditors said VA was on track to lose more than $261 million over five years on treatment and supplies that veterans would not use.
Two years later, McDonough announced he had a plan.
Changes and backlash
The proposal pending in the Federal Register takes into account – for the first time – sleep apnea’s responsiveness to treatment. Fully treated, the condition would be rated at zero percent, as would an asymptomatic case, and the current 30 percent rating would be eliminated.
VA would assign ratings above 10 percent only when treatment is ineffective or isn’t advised because of another ailment. And a 100 percent rating would be granted only in rare cases, when the disorder compromises vital organs.
The new rules would “incorporate modern medical data and terminology to provide Veterans with more accurate and consistent decisions,” McDonough said in a statement at the time.
VA would still pay for veterans’ medical care, as well as CPAPs and other devices. But it would impose more stringent requirements to prove that apnea causes significant limitations beyond fatigue. To qualify for benefits, overweight veterans would need to show they had tried to lose weight to manage the condition.
The proposed updates would also put guardrails around PTSD and tinnitus. These commonly claimed conditions afflict many veterans, from troops who served stateside to those who deployed to combat zones. But because diagnoses for both disorders rely on self-reported symptoms, disability experts say they are vulnerable to exaggeration or fraud.
About 34 percent of veterans received disability benefits in 2024, up from 9 percent in 2001. In that time frame, the veteran population decreased by a third.
Since 2003, tinnitus has ranked as the most commonly compensated claim, with 3.2 million awards last year alone, according to VA data. More than half of veterans with a disability rating received benefits for the condition. Tinnitus carries a relatively low rating, at 10 percent, but is often touted by for-profit companies and influencers as a step toward achieving a 100 percent rating.
Tinnitus would be downgraded from a stand-alone condition to an underlying symptom of hearing loss – a change that critics say would jeopardize the benefit for many veterans who suffer from it.
Meanwhile, more than 1 in 4 disabled veterans, or nearly 1.6 million, received monthly compensation for PTSD last year, a nearly elevenfold increase since 2001, according to VA data. The proposed rules would modernize how this and other mental health conditions are evaluated, emphasizing the disorders’ disruption to a veteran’s life, rather than on their professed feelings of anxiety and depression alone.
Still, the new rules would also result in higher payments to some veterans, and the minimum rating for mental health ailments would rise from zero to 10 percent.
Federal law required VA to consider public comments for and against the proposed changes for 60 days after they were published in the Federal Register.
Among the 2,700 comments were those from veterans who said they would stop treating their sleep apnea if it meant their monthly check would be cut.
“This is absolutely ridiculous, how do you people sleep at night?” one commenter who identified herself as a veteran wrote. “Definitely without a mask or sleep apnea that’s for sure.”
Another wrote, “I am just appalled that every time I try to submit a claim, the VA tries to pass something that takes away from the combat veterans.”
Major advocacy groups, including VFW and the National Organization of Veterans’ Advocates, issued blistering statements accusing VA of relying on inaccurate or dated research to justify the changes. The American Tinnitus Association assailed the plan as “a blatant attempt to reduce costs at the expense of our Veterans with tinnitus who depend on and deserve disability benefits.”
As VA keeps the door open, for-profit claims companies and VA staff alike are urging veterans to maximize their benefits.
Brian Reese, the founder of VA Claims Insider, warned his more than 155,000 YouTube subscribers in an August video to act with urgency and “file your claim immediately” before any changes take effect.
Inside the Veterans Club at the Sturgis Motorcycle Rally in South Dakota in August 2024, Randy Schmitz was intrigued when a VA employee made the rounds, asking whether any veterans wanted to file for disability benefits. Schmitz, 65, said he has used a CPAP machine since he was diagnosed with sleep apnea a few years after leaving the Navy in 1987. But he never filed a claim for it.
“I thought you couldn’t get coverage if you had surgery or if you get a machine, because it cures you,” he told the staffer, Jamie Agorua.
Twenty minutes later, he was in an air-conditioned trailer meeting with Rebecca Halterman, a claims reviewer with the benefits administration. She opened her laptop to search for his military record.
Yes, she told Schmitz: VA would probably provide his CPAP free and compensate him generously for sleep apnea.
He decided to file a claim for it and for a few other conditions. A shop foreman for the county in Carlton, Minnesota, Schmitz was already receiving a modest disability check each month for hearing loss and tinnitus.
But Halterman told him there was more on the table. She was happy to hear that he was open to pursuing more from the government.
“Honestly, where have you been, sir!?” she asked him. “Not coming to see me!”
Early this year, VA turned down Schmitz’s sleep apnea claim. Benefits officials told him there was insufficient evidence in his Navy record that he had sought help for the condition while in the service, he said – “and there was absolutely no sleep tests or anything to treat me back then.”
He’s determined to try again. Schmitz said he is attempting to get in touch with a sailor he served with, hoping he will write a buddy letter about Schmitz’s snoring. Then he plans to contact his local representative for Disabled American Veterans to file a new claim.
Top Articles in News Services
-

Arctic Sees Unprecedented Heat as Climate Impacts Cascade
-

Prudential Life Expected to Face Inspection over Fraud
-

South Korea Prosecutor Seeks Death Penalty for Ex-President Yoon over Martial Law (Update)
-

Trump Names Former Federal Reserve Governor Warsh as the Next Fed Chair, Replacing Powell
-

Japan’s Nagasaki, Okinawa Make N.Y. Times’ 52 Places to Go in 2026
JN ACCESS RANKING
-
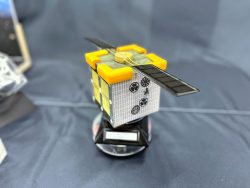
Univ. in Japan, Tokyo-Based Startup to Develop Satellite for Disaster Prevention Measures, Bears
-

JAL, ANA Cancel Flights During 3-day Holiday Weekend due to Blizzard
-

China Confirmed to Be Operating Drilling Vessel Near Japan-China Median Line
-

China Eyes Rare Earth Foothold in Malaysia to Maintain Dominance, Counter Japan, U.S.
-

Japan Institute to Use Domestic Commercial Optical Lattice Clock to Set Japan Standard Time